Are You A Lactation Consultant Looking for Dr. Nice’s Moisturizing Gel?
You’ve Come to the Right Place!
Dr. Nice’s Moisturizing Gel is the only lanolin-free, vegan, peppermint nipple gel that soothes sore, cracked, and chafed nipples on contact! Our all-natural formula is safe for Mom and Baby, so there’s no need to wash it off before breastfeeding.

Dr. Nice’s Moisturizing Gel is…
Lanolin FREE
Water Based
Vegan
Pharmacist Formulated
Soothing & Cooling
Safe for Mom & Baby
WHO Code Compliant
USA Made
If you’re interested in purchasing Dr. Nice’s Moisturizing Gel wholesale for your practice, please reach out to our Sales Team at [email protected].
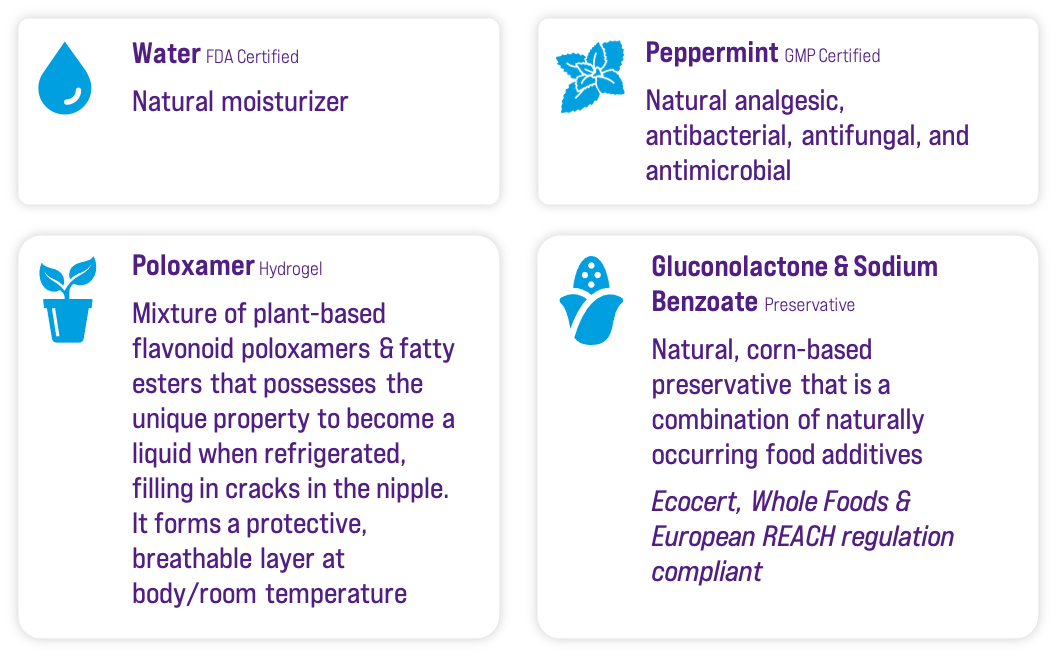
All-Natural Ingredients
How to Use Dr. Nice’s Moisturizing Gel for
Instant Soothing Relief on Painful, Cracked Nipples
USE A SMALL AMOUNT AND APPLY IN A THIN LAYER … A LITTLE GOES A LONG WAY!
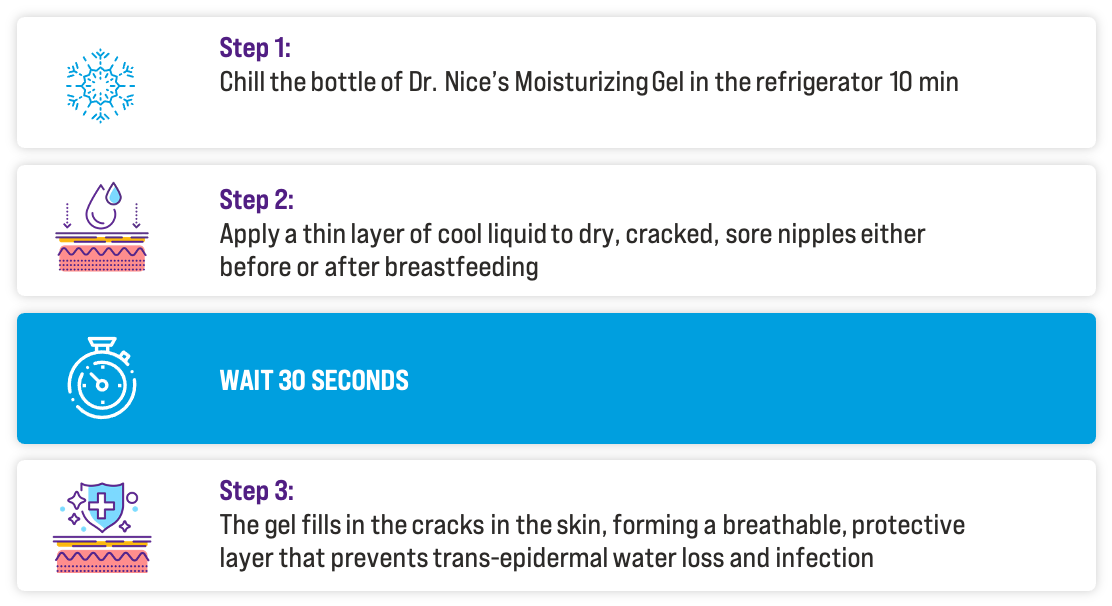
IF THE GEL DRIES WITH A WHITE APPEARANCE, TOO MUCH WAS USED.
SIMPLY RINSE OFF WITH WARM WATER, DRY AND REAPPLY A SMALLER AMOUNT.
Books by Dr. Frank J. Nice
All proceeds from the sales of Dr. Nice’s books and a portion of the proceeds from the sale of Dr. Nice’s Moisturizing Gel supports the work of the non-profit humanitarian relief organization, Health and Education for Haiti. Learn more at hehonline.org.
The breastfeeding family’s guide to nonprescription drugs and everyday products

A must-have reference guide for all breastfeeding parents. A truth regarding breastfeeding and everyday products.
THE GALACTAGOGUE
RECIPE BOOK
Over 200 recipes featuring major and minor galactagogues-certain foods and herbs that likely increase prolactin or oxytocin to initiate the breastmilk letdown reflex, helping to increase production.
RECREATIONAL DRUGS AND DRUGS USED TO TREAT ADDICTED MOTHERS

Provides a rational framework that can successfully guide clinical decision making on the impact of certain drugs on pregnancy and breastfeeding.
Reference Materials for Lactation Consultants
Looking for an answer to a pharmacology question or dosage guidelines for your breastfeeding clients?
Dr. Frank J. Nice has put together a free collection of information, recommendations, and advice for Lactation Consultants to use in their practice.

Questions? We’d love to hear from you.
If you have breastfeeding and/or lactation questions, we’d love to hear from you! Please reach out to us via the email below.
Proudly Made in the U.S.A. in San Diego, California
Let’s Get Social!